Choosing the right baby toys 0–3 months supports early sensory, motor, and cognitive development. With a few safe, simple items—and lots of loving interaction—you can make the first three months calm and engaging.
Best Baby Toys 0–3 Months for Early Development
Newborns see best at 8–12 inches and respond strongly to high-contrast patterns, gentle motion, and soft sounds. These baby toys 0–3 months are ideal starters:
- High-contrast flash cards / soft cloth books – bold shapes help visual focus and tracking.
- Soft rattles – light sound + easy grasping encourage early cause-and-effect.
- Crib mobile – slow, gentle movement invites calm attention before sleep.
- Baby mirror – babies love faces; safe mirrors spark curiosity.
- Baby play mat – a comfy base for tummy time and motor practice.

High-Contrast Cards or Soft Cloth Books
How to use: Hold cards 8–12 inches from baby’s face during awake time or prop one during tummy time. Rotate a few patterns to keep it fresh.
Choose non-toxic inks and soft, rounded edges. Cloth books should be washable and colorfast.
Soft Rattles
How to use: Shake once or twice, pause, and wait for baby to look back. Wrist rattles help babies “find” the sound source earlier.
Crib Mobile (with Gentle Music or Motion)
How to use: Keep out of reach; limit to 10–15 minutes to avoid overstimulation. Remove once baby can push up or sit.
For nursery safety basics, see this concise NHS overview.

Baby Mirror
How to use: Place a tummy-time mirror on the play mat; sit face-to-face and talk about what baby “sees.”
Baby Play Mat
How to use: Start with 2–3 minutes several times daily; add a high-contrast card within view to extend interest.
How to Play: Tiny Routines That Work
- Tummy time: start with 2–3 minutes, a few times daily; prop a high-contrast card within view. Helpful pediatric tips on tummy time.
- Mobile moments: 10–15 minutes before sleep to cue wind-down—avoid overstimulation.
- Sound play: shake a soft rattle, then pause; let baby process and look back.
- Texture time: offer a crinkle toy or comfort cloth; narrate what baby feels.
Your voice is the “best toy.” Short, calm narration of what baby is seeing or hearing boosts bonding and language foundations.
Safety Notes
- Check for choking hazards: no small detachable parts; seams secure; materials non-toxic and washable.
- Mobiles must remain out of reach; remove as soon as baby can push up or sit.
- Avoid overstimulation—dim lights, soften sounds, and keep sessions short.
For age-appropriate toy advice, see the American Academy of Pediatrics’ toy guidance, and CDC infant milestones here.
Optional (Soon): Toys for 3–6 Months
- Sensory ball – textured surfaces invite grasping and hand–eye coordination (often 3–6 months).
- Teething ring – typically helpful after 4–6 months when teething discomfort starts.
Conclusion: A Calm Start with Baby Toys 0–3 Months
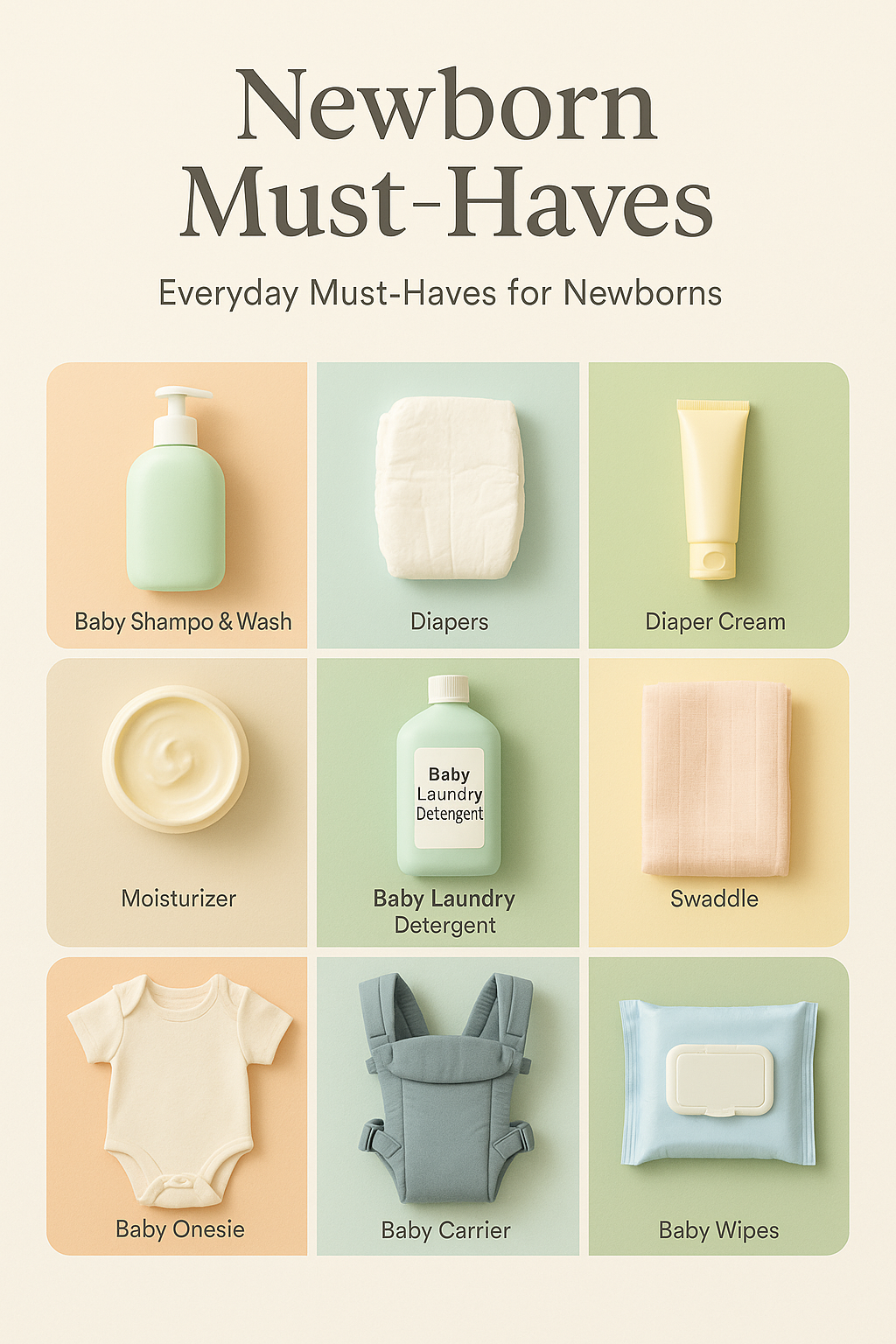
A handful of safe, simple baby toys 0–3 months—plus your voice and eye contact—are all your newborn needs. Keep play gentle, rotate a few favorites, and enjoy tiny milestones. For smoother days and nights, try our Gentle Newborn Sleep Schedule, and if you’re still prepping for baby, see the Newborn Must-Haves Checklist.

📌 You May Also Like
For more on safe play, see AAP toy guidance and early milestones at the CDC.
This article is for informational purposes only and isn’t a substitute for personalized medical advice from your pediatrician.